Overview – what is lipoedema?
Lipoedema is a long-term and complex condition that almost exclusively affects people assigned female at birth and leads to an uneven increase in adipose tissue (fat) mainly in the hips and legs, and sometimes the arms It is usually symmetrical with both limbs affected equally but it does not affect the feet or hands, this can lead to a bracelet effect at the ankle or wrist. Tenderness and pain are common in affected areas. The skin may look more floppy or dimpled in the affected areas.
The change in shape usually starts in weight gain at times associated with hormonal changes, such as puberty, pregnancy and menopause.
We do not know how many women have lipoedema as it is often misdiagnosed and confused with obesity and lymphoedema.
Symptoms – what are the signs symptoms of lipoedema?
Lipoedema seems to be a syndrome with various symptoms reported but not all necessarily present in each case. The main presenting signs are fat tissue changes affecting the legs and sometimes the arms, which may cause the body to look out of proportion. The condition usually presents symmetrically but the hands and feet are not affected. There may be fat “bulges” which develop around the knees or hips.
It can be present for a number of years before symptoms of pain or the feeling of severe heavy legs may occur, at which point the condition may lead them to ask their health care professional and it may be suggested they have lipoedema.
It is thought that the pain experienced by people with lipoedema is related to inflammation and reduced oxygen to the tissues. Unfortunately, there is no test you can undergo to diagnose lipoedema, therefore not a lot of research exists about it.
Bruising and thread or varicose veins are another symptom associated with lipoedema but as yet there is no physiological explanation for this.
Often there is associated joint pain reported and this may impair mobility. This can be more problematic if obesity is co existing.
There is no evidence of oedema / swelling in lipoedema but it is possible to have lipoedema and also suffer from lymphoedema / chronic oedema which may be related to obesity or other conditions such as vein disease.
It is not thought that lipoedema leads to weight gain but gaining weight does make the symptoms of lipoedema (pain and heaviness) worse.
What does lipoedema look like?
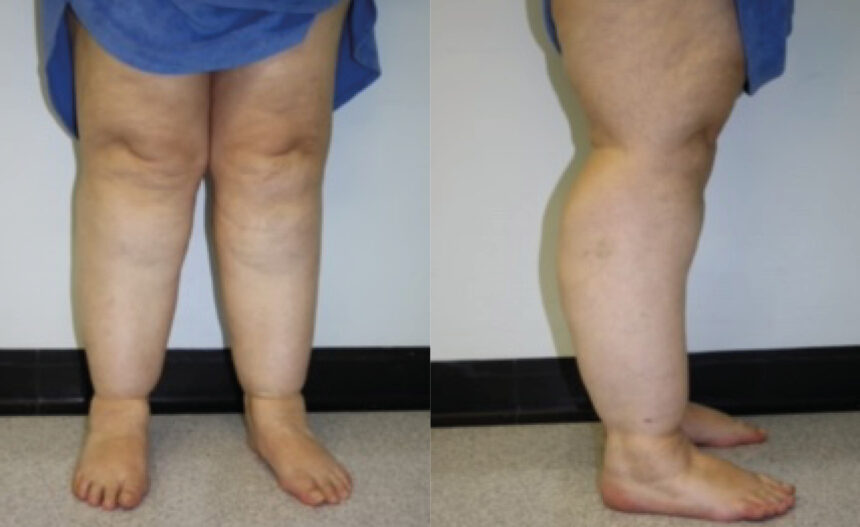
Lipoedema results in a change in body shape due to the abnormal distribution of adipose tissue ( fat) in legs, hips and sometimes the arms, which is out of proportion with the rest of the body. There is often associated pain and tenderness in the tissues. The skin may also be altered with the skin feeling cooler and have a more “floppy, dimpled” appearance. People living with lipoedema often report they bruise more easily but there is no known physiological reason for this. Mobility may also be more difficult if the legs are heavy.
Watch our film to hear from Emily a sufferer of lipoedema
Causes of lipoedema
We do not know the cause of lipoedema or what makes someone more prone to developing this condition. Hormonal factors are thought to contribute to the condition but there is no evidence that any tests would detect any abnormalities.
Research appears to show that weight gain is most likely to make the condition worse if someone is likely to develop lipoedema.
Diagnosis of lipoedema
A health care professional, such as a lymphoedema practitioner, will help to decide if lipoedema is an appropriate diagnosis. As there is no test which can be undertaken the diagnosis will be established by the history given and the presentation. Lipoedema is often misdiagnosed.
Treatment – what treatment will I be offered for lipoedema?
As with all long term conditions the treatment for lipoedema will encourage establishing the best treatment plan for that person and giving them the strategies to be experts in their own self management.
Reduce / maintain healthy diet and body weight
People with lipoedema can often be overweight, so to reduce the symptoms of lipoedema and prevent it becoming worse, it is important to maintain a healthy diet and weight (rather than dieting for weight loss). If very overweight, those with lipoedema should seek professional advice from their primary care professional.
Focus on increasing your activity / movement.
It has been shown that regular exercise can reduce inflammation and it increases blood flow and oxygen in the adipose tissue (fat). Exercise can help reduce the symptoms of pain and heaviness in the legs as well as being good for our mental well-being. It can help strengthen muscles which will protect the joints and hopefully reduce the joint problems some people living with lipoedema experience. Many people with lipoedema say their symptoms are improved with swimming or water aerobics.
Wear compression
Compression therapy may have an anti-inflammatory effect on the tissues and can improve microcirculation so wearing compressive sportswear, lycra-style leggings or compression hosiery can make your legs feel more comfortable. However compression will not reduce the amount of fatty tissue or prevent an increase in fat if you gain weight. Some people may need medical compression garments provided by a health care professional.
Liposuction
In March 2022, the national Institute of Clinical Guidelines (NICE) concluded that there is not enough evidence to support recommending liposuction for lipoedema, and it should only be undertaken as part of a research project. Consequently, some sufferers are seeking treatment overseas. Anyone considering this is advised to read the NICE 2022 guidance, research the surgical team undertaking the procedure and consider the practicalities of post-operative support available and visit the Lipoedema UK website.
If you think you have lipoedema or if you feel that your mental health is affected by lipoedema you should get in touch with your primary health care professional.
Outlook for lipoedema
Lipoedema is a long term condition which at present is able to be managed by the individual with input from a healthcare professional as required but is not curable.
Prevention of lipoedema
As the cause for lipoedema is not established it is difficult to prevent this condition. However, for those predisposed, maintaining a healthy weight is the best method of preventing worsening of the condition.
Harm – the risk factors
- Failing to recognise lipoedema as a condition / dismissing patients as just being obese causes substantial psychological harm, particularly as it tends to arise at times in the life cycle when people are vulnerable, for example during puberty
- Encouraging severe weight loss in someone with lipoedema may cause nutritional imbalance
Resources
Talk Lipoedema (website link)
Other support
Some organisations you can contact for further information.
Accelerate Based in East London, Accelerate can accept national referrals from your GP / specialist to our world-class centre where we pioneer and trial experimental new treatments for chronic leg ulcers / wounds, lymphoedema and mobility challenges.
Contact details
020 3819 6022
hello@acceleratecic.com
Find out more on the Accelerate website
Lipoedema UK Their focus is to educate doctors, health professionals and the public about Lipoedema and its symptoms, so it may be diagnosed and treated earlier. They believe that with earlier diagnosis and treatment women can prevent developing further complications and manage their Lipoedema.
Contact details
info@lipoedema.co.uk
Find out more on the Lipoedema UK website
Royal College of Podiatry The Royal College of Podiatry exists to ensure the public has access to high quality foot care delivered by qualified and regulated professionals.
Contact details
020 7234 8620
reception@rcpod.org
Find out more on the Royal College of Podiatry website
Diabetes UK Diabetes UK are the leading UK charity for people affected by diabetes it’s their responsibility to lead the fight against the growing crisis. And this fight is one that involves all everyone – sharing knowledge and taking diabetes on together.
Contact details
0345 123 2399
helpline@diabetes.org.uk
Find out more on the Diabetes UK website
Tell us what you think
If there’s anything you want to ask us or tell us, whether it’s a suggestion about our website, a complaint, or a compliment, drop us a line at
support@legsmatter.org