Your response to this question may be to ask, ‘What changes in leg ulcer management? What am I missing?’ The dispiriting answer is that for leg ulcer management, unlike for so many other physical conditions, for many years little has changed.
Look at stroke, heart disease, diabetes… In the last 20 years there have been significant improvements in our clinical understanding and technological advances. Not so with leg ulcers. So you are not missing anything new and fancy, despite the rare article in the Daily Mail. This is a very sad state of affairs for a clinical condition that makes up over 40% of district nursing time.
Good leg ulcer management should be delivered through a fantastic and joined up system, where effective compression therapy is delivered promptly and consistently by a few regular skilled practitioners, where patients who are already more complex are flagged and there is a pathway for community focused medical management, within a system that supports patients in full time work with flexible appointments.
It goes without saying that this type of well organised pathway would improve lives and prevent years of suffering. And this is one condition where effective and early care really does save money for the local health economy too. But what do we have? There will be a few areas where the above ideal scenario is in place, but very few.
Talking about harm
What we see in the UK are all the hallmarks of a system that is failing the people it is meant to serve. We need to name this as harm and stop dancing around the issues. We have nursing vacancies that stop consistent care or a timely ABPI*, we have increased use of light compression across the UK slowing the path to healing and poor understanding of the impact of pain on lives or tolerance of treatment.
Many patients who are employed can lose their jobs whilst trying to attend clinics in the afternoon regularly. And Tissue Viability nurses spend all their hours on the industry of pressure ulcer management and reporting. Community nurses feel impotent to change this and bear the brunt of the impact on their own working lives; the following scenario is too common.
Case study
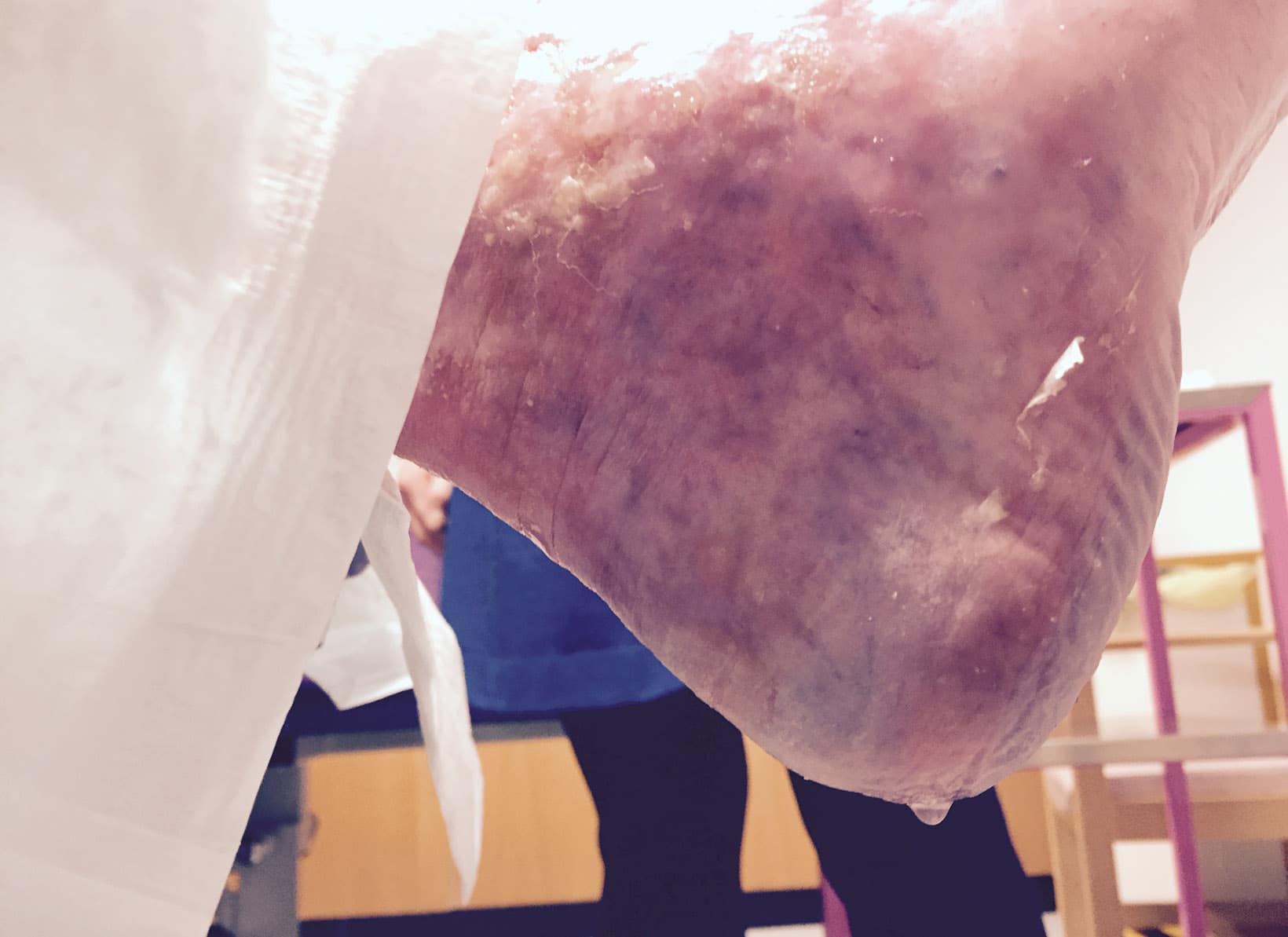
A simple pretibial trauma created uncontrolled exudate, creating a vicious cycle of excoriated skin, terrible pain, massive use of absorbent dressings, daily District Nurse visits and ruined footwear and bedding. You know the scenario. Why has she had this for 8 months? Because to have an ABPI was too painful and the local guidelines and the Tissue Viability Nurse said, ‘no Doppler, no compression’. There are good reasons for these guidelines, but sometimes the ‘Computer says no’ response needs unpicking. By accepting and not critiquing the impact, this created harm.
Realistically, how much worse could it be for her? The unmanaged oedema was ruining her leg and life. With a palpable pedal pulse she responded to light compression with oversight of the possible risk. It was a simple focus on ‘what do we do to stop the dripping?’ She thought we were miracle workers; I knew differently.
What is interesting about the harm that this creates for people with ulcers and their families is that this also has a terrible impact on the morale of the community nurses who care for this group day in, day out. Visiting someone daily to change dripping bandages is incredibly demoralising, knowing that whatever you do, it will be like this tomorrow. It’s even worse for everyone if they are in significant pain. And of course daily dressings take up an enormous amount of time, especially when there is no end in sight.
I am not saying that we ignore guidelines and just compress without assessment. What I am suggesting is that we need to critique the current state of management across the UK, that we should not accept how things are or have such low expectations that this can change.
Legs Matter
There is a coalition of organisations and societies who have said, enough is enough, that leg ulcer management needs to change and we need to recognise that what is happening for people is actually harm. That we know what is needed and this needs to be implemented. 20 years’ worth of ad hoc clinical education has not created the change required so we will aim our sights on raising the expectations of patients first, then clinicians. This coalition is called ‘Legs Matter’ and we will be launching the campaign in April 2018 at the Tissue Viability Society annual conference.
So to get back to the question, if you are not seeing any changes in leg ulcer management, how is this affecting you, your team and your patients? How many patients are on your caseload for daily or alternate daily dressings? And why? What can you and your team do about this?
About the author
Alison Hopkins is CEO of Accelerate, a social enterprise specialising in wound and lymphoedema management. Alison remains a clinical expert in community focussed Tissue Viability, having started out as a District Nurse.
*Ankle-brachial pressure index
Source
The original article featured on the Queen’s Nursing Institute website.









