A Legs Matter webinar delivered in partnership with Flen Health ![]()
Summary
We must be compassionate as to how we manage wound care consultations to ensure that we see the person before the disability. Also, to enable personalised gold standard care we must begin to build a body of evidence to know how best to support this group of people living with leg and foot wounds.
3 steps to take to best support people with a learning disability in managing their wound care
- Get to know your patient and listen to their needs
- Offer reasonable adjustments to personalise their care
- Keep up to date with the legislation and professional standards with both mandatory and non-mandatory training
What you will learn if you watch the webinar
World Health Organisation “engage the patient’s voice”
Ciara Lawrence, campaigner from Mencap and a person living with a learning disability opened the discussion agreeing that she supported the 2023 campaign by The World Health Organisation (WHO) ‘engaging patients for patient safety’, and to ‘engage the patient’s voice’.
The WHO’s objectives for their global patient safety action plan are to:
- Raise awareness
- Engage policy makers
- Empower patients and their families
- Advocate urgent action
Legs Matter agree that we need to make a change in the way we support patients with leg and foot wounds.
Learning Disability Register
Ciara explained about something that had made a big difference to her was to have her medical record identified with the learning disability register. This was because this initiates, from point of contact with her health and care teams, an awareness that she may require reasonable adjustments to be made at her appointments.
Examples of reasonable adjustments might be:
- An increased length of appointment time
- Use of easy read materials
- Music therapy
- Having a friend or family member in the consultation.
The panel agreed that this would be an easy step in the right direction to support those living with a learning disability and would go some way to reduce health inequalities and improve health literacy, in support of personalising care.
Are people with a learning disability being harmed in their wound care consultations?
Well, “we just don’t know” advised Dr Lindsey Cherry. There is very little research to inform us either way, but being data poor would suggest that it is likely that there is a potential. This is something that 70% of the webinar listeners, during an online poll, agreed with.
We believe that healthcare workers do not deliberately go out to inflict harm on those under their care, so what can we do to be more informed? Lindsey, explained that building evidence through clinical case studies, collecting data and carrying out an audit to evaluate our practice would be a great place to start. She explained that more research needs to be done to develop our awareness in support of wound care within the social model of care for those people with a learning disability and that this would ensure inclusivity of the health and care offering.
Professional stardards and duty of care
As health and care professionals we have a duty of care to best support those people with protected characteristics under the Equality Act, 2010; and there are professional standards written into regulatory registration which health care professionals sign up to on revalidation of their professional integrity.
Martin Furlong highlighted that it is important that we maintain those high standards to ensure inclusivity and prevent harm to anyone in our care. It is not always easy to provide gold standard care in the traditional sense because gold standard is what is right for the recipient of the care at the right time based on informed knowledge. Therefore, it is good practice to make reasonable adjustments and to be mindful of external factors such as culture and tradition, friend/family support or if the environment in which the care is being provided is suitable or familiar.
All this can make a difference to the understanding and outcome of the care provided and it is important to make good clinical notes to inform the circumstances surrounding the treatment or advice provided.
Lindsey added that the offer of time and the use of open-ended questions such as ‘what would you like to know?’ within the consultation might make a difference, enabling a comprehensive awareness of what was required for both the clinician, the recipient of the care and their care network.
How ready are we as clinicians to allow the care recipient to guide a consultation and make their own decisions
Ciara agreed that she would want her clinician to allow her to feel involved in her treatments and felt the offer of more time within the consultation would be a high priority to enable meaningful conversations for those with a learning disability; as would the use of other forms of communication for those who might be non-verbal such as the use of Makaton or for those with reading limitations to have easy-read, video or speech information assets available.
Where to access training for those working with people with learning disability and autism
The Oliver McGowan training on learning disability and autism, is available on the NHS e-learning for health (e-lfh) website is mandatory for all working in public services like the NHS and highly recommended for those in privately funded establishments. The Personalised Care Institute have a wealth of online information and education for health and care workers on how to involve patients in making decisions around their care. The TUC offers education for trade union representatives to inform and support the workplace both for employers and employees.
Moderator
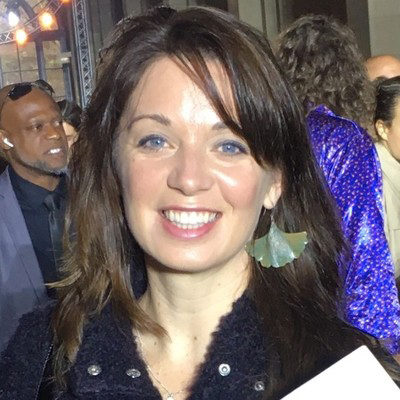
Joanne Casey – Professional Development Lead, Royal College of Podiatry (RCPod)
Speakers
Dr Lindsey Cherry – Associate Professor of Personalised Care, University of Southampton and Podiatrist, Central Southampton Primary Care Network
Lindsey has authored 50+ papers, several book chapters, and is a member or chair of various national and international committees.

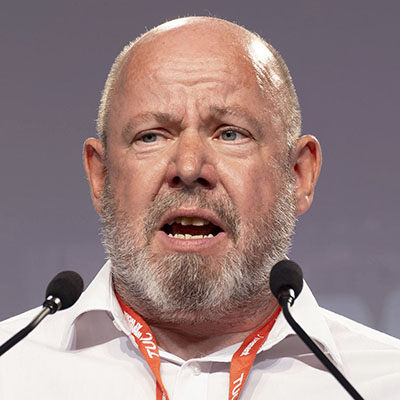
Martin Furlong – Head of Employment Relations at the Royal College of Podiatry (RCPod)
Martin worked previously as a union officer in the airline industry, telecoms and the civil service before moving onto to his current role covering members in the NHS and private healthcare. Prior to becoming a trade union officer Martin was a lay rep for many years in the finance industry and joined a union on his first day at work in 1982.
At RCPod he leads on all employment and EDI issues as well as heading up the team dealing with Professional issues in Podiatry.
Ciara Lawrence – Engagement Lead at learning disability Charity Mencap

Ciara has lived experience of a learning disability. Her work involves talking and listening to people with a learning disability to make the work of Mencap more inclusive. She is an Ambassador for Grace Women charity, Eve Appeal and Jo’s Cervical Cancer Trust and Patron of Dance Syndrome and Trustee for Sunnybank Trust and is also a Podcaster.
Her Podcast ‘Ciara’s Pink Sparkle aims to help challenge attitudes about people with a learning disability in an accessible way and includes some star guest interviews!









