Overview – non diabetes related foot ulcers
We all get wounds on our feet, sometimes from shoes that have rubbed or by injuring our feet in some other way.
If you do not have diabetes and you have a wound on your foot, then you should seek advice from your healthcare professional if your wound is not showing signs of healing within a week. This might be a sign of an underlying problem that needs investigating further.
If you have a non-healing wound on your foot, it is possible this may be caused by peripheral arterial disease (poor blood flow to the feet), which is a known complication of other illnesses such as heart disease.
Some people have loss of sensation or feeling, within their feet caused by nerve damage (neuropathy). This could mean that you may not notice if you injure your feet
Skin damage to the feet can also be caused by accidents or friction. It may cause a wound or break in the skin, or blistering which could also lead to a wound (ulcer).
Less commonly, wounds on the feet can also be caused by venous disease (such as varicose veins). More rarely, ulceration might be due to a skin cancer so should be seen to promptly.
Symptoms – what are the typical symptoms of non diabetes related foot ulcers?
Some people may not feel the symptoms of foot ulceration (including pain) due to neuropathy (nerve damage) that may be present. As a result, people with foot ulcers that become infected may feel generally unwell (flu-like symptoms, fever, chills, nausea) before they realise that there is a problem. Infection is common across all types of ulceration, and may rapidly through the foot resulting in major tissue destruction.
The signs of a red (although this may not be present in pigmented skins), hot, swollen foot, with or without pain, should not be overlooked as the progression from an initial minor injury to unsalvageable tissue damage can be rapid.
What do foot ulcers look like?

Non diabetes related foot ulcer

Causes – what can cause non diabetes related foot ulcers?
Peripheral arterial disease
Reduced blood flow to the foot means the skin can become thinner and weaker, and more prone to damage from rubbing or friction. Any break in the skin can then develop into an ulcer. One cause of poor healing in the lower leg is when not enough blood is getting to our feet. Blood travels from our heart to our feet through our arteries. It carries oxygen and nutrition to the skin and deeper structures. If our arteries become too narrow or blocked, our skin will not get enough blood to allow the wound to heal as normal.
Arteries can become ‘furred’ up by the build-up of fibrous and fatty material inside the arteries (atherosclerosis). Atherosclerosis is the underlying condition that causes cardiovascular disease, such as heart attacks and strokes, as well as affecting the arteries that supply the legs. This is called peripheral arterial disease.
You can read more about peripheral arterial disease on NHS Choices and on the British Heart Foundation website.
Diagnosis – getting diagnosed with a non diabetes related foot ulcer
Self care
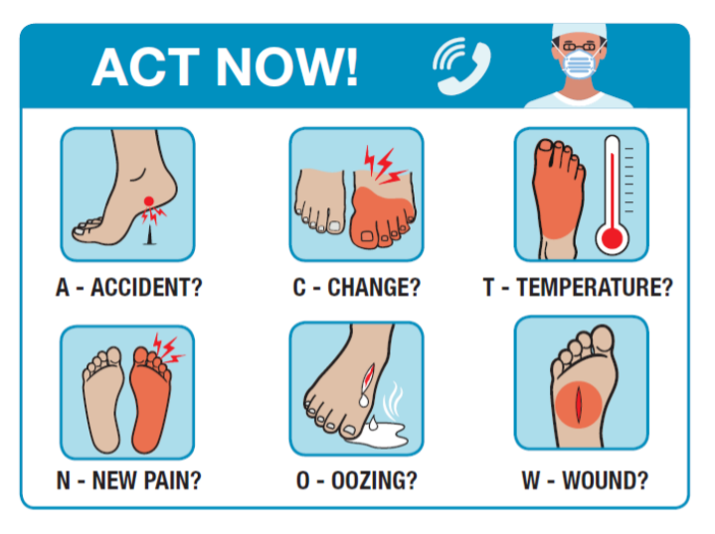
Self checks may identify problems with your feet . Look for the following warning signs that may result in ulceration and help you know when to seek a referral to specialist care:
- Accident resulting in a cut or break to the skin
- Change to normal appearance
- Temperature – change in temperature
- New pain
- Oozing
- Wound
Treatment – how do you treat a non diabetes related foot ulcer?
Making an appointment
If you have a wound on your foot that is not healing, make an appointment at your GP practice or with a podiatrist. You may be given an appointment to see the nurse rather than the doctor as they (and podiatrists) are often responsible for caring for patients with leg and foot problems.
When you see the nurse, podiatrist, or doctor, they should:
- Ask about your symptoms and how long you have had problems;
- Examine your lower legs and feet;
- Check your circulation by palpating your pulses, listening to your pulses with a Doppler. They may also take pressures around your arm, ankle and toe. This test compares blood flow to find out if there are circulation problems in your lower leg. You may have to come back to have your Doppler test on another day or at another clinic but if this test is required, you should have this test within a few weeks of your first appointment
- Test whether you have any loss of sensation in your feet
You might also be offered some more tests (for example, blood tests) to rule out other health problems that can affect your legs and feet, including diabetes, anaemia, thyroid, kidney and cholesterol problems.
If your GP practice thinks you have problems with your arteries, they may refer you for further vascular tests at your local hospital or specialist clinic for opinion and intervention regarding blood supply to the legs and / or feet.
What to expect at your appointment
Most people with a non-healing foot wound need to be urgently referred to a podiatrist who will act as the gatekeeper to the wider multidisciplinary healthcare team.
You should have an initial assessment that includes an examination of both feet to look for evidence of:
- Neuropathy (nerve damage) – using a nylon filament t as part of a foot examination to check the feeling in your feet
- Assessment of the blood flow to review whether you need referral to a vascular specialist (see the NICE guideline on lower limb peripheral arterial disease)
- Ulceration
- Callus (hard skin)
- Infection and / or inflammation
- Deformity
- Tissue damage or gangrene
- Charcot arthropathy (a rare complication of nerve damage which can affect the bones)
- Scleroderma
- Venous disease and Atrophie Blanche in particular
If you need to have further assessment, this should include:
- Doppler assessment of ankle brachial pressure index and / or toe pressures
- X-rays or other scans to determine any deep tissue (eg bone) involvement
- Microbial culture (wound swab or tissue sample)
- Gait analysis which includes looking at the way you walk
- Pressure mapping
Referral options for diabetes foot ulcers
You may be referred to a specialist podiatrist and / or vascular service if your foot ulcer is not healing. Treatment should include these six main components for any foot-related wound to optimise the chance of wound healing:
- Management of the underlying condition or cause eg, optimising blood flow, management of any excess fluid (oedema) etc
- Debridement of the wound. This is the removal of material from within and around the wound such as slough, biofilm and callus which can impede wound healing
- Good management of wound symptoms through appropriate dressing selection or adjunctive therapies
- Managing infection
- Offloading or deflecting pressure away from the wound. This may involve shoe adaptations, inserts (insoles) or orthopaedic walkers are required
- Compression therapy may be required for some tyles of leg / foot ulceration where peripheral arterial disease has been excluded
Appropriate footware and podiatry visits
If you have ever been diagnosed with a chronic foot wound, you should be placed into a protective foot care programme. It is important that you have regular podiatry visits, footwear and orthotic reviews, and that you receive the most appropriate recommended medical management (such as medicines to control your cholesterol levels, blood pressure and to reduce the ‘stickiness’ of your blood).
If you have peripheral arterial disease and a foot wound, you may be at increased risk of cardiovascular incidents such as stroke and heart attack and should have your cardio-vascular risks modified.
Prevention – how to prevent a non diabetes related foot ulcer occurring or reoccuring
There are lots of things you can do to help prevent foot ulcers:
- Daily self checks
- Ensure that your footwear is right for your foot shape (seek advice if needed)
- Maintain a healthy lifestyle
- No smoking (if you smoke, stopping smoking is probably the single most important thing you can do. Help and support to do this is widely available)
- Detect any foot problems early and avoid delays in seeking specialist advice and treatment
- Take all medications as prescribed. Speak to your GP or pharmacist (or the person who has prescribed your medicines if your are not sure why you have been prescribed them, or how you should be taking them)
Outlook when you have a non diabetes related foot ulcer
You may be affected by a foot ulcer as some point during your life. If you delay in seeking specialist treatment, this can lead to an increase in poor outcomes, such as:
- Infection
- Amputation
- Disability
There is always a risk of recurrence of a foot problem once you have had an initial ulcer, so there is a need for ongoing vigilance.
Foot ulcers do not just affect feet, they can have an impact on your overall health and they may, in some people, lead to a shortening of life.
Harm – the risk factors for non diabetes related foot ulcers
Failure to take prompt action if you have a foot ulcer can cause harm.To help prevent more serious problems, make sure that you:
- Regularly check you feet and legs
- Attend your scheduled podiatry appointments
- Seek advice if you have any non-healing wounds on the feet (within 7 days)
- Wear good fitting, supportive footwear
- Take antibiotics and other medicines as prescribed
If you have any concerns about the treatment or care you are receiving, it is important to discuss with your health care professional or seek further advice.
If you have any concerns about the treatment or care you are receiving, it is important to speak up.
Resources
- ACT NOW foot assessment tool (Web page)
- Diabetes UK: Putting Feet First campaign (Web page)
- Touch the Toes Test to test for sensation in the feet (PDF download)
- DESMOND, self-management education programme for people with Type 2 diabetes (Web page)
- The NHS and its partner Diabetes UK are delivering a new programme which provides a low calorie, total diet replacement treatment for people who are living with type 2 diabetes and obesity or overweight: the NHS Type 2 Diabetes Path to Remission Programme (Web page)
- Top tips for foot care (PDF download)
- Tips on choosing the right footwear (Web page)
Clinical guidelines for foot ulcers
- NICE Peripheral Arterial Disease Diagnosis and management (Web page)
- NICE Guidelines for the prevention and management of the Diabetic foot (Web page)
- Scottish intercollegiate guidelines on diabetes (PDF download)
- Best practice guidelines. Wound management of diabetic foot ulcers (PDF download)
- Local management of diabetic foot ulcers (PDF download)
Research
- The Cochrane Library publishes systematic reviews about the effectiveness of many treatments for diabetic foot ulcers and summarises this in a useful
- ‘Evidently Cochrane’ paper (Web page)
Other support
Some organisations you can contact for further information.
Accelerate Based in East London, Accelerate can accept national referrals from your GP / specialist to our world-class centre where we pioneer and trial experimental new treatments for chronic leg ulcers / wounds, lymphoedema and mobility challenges.
Contact details
020 3819 6022
hello@acceleratecic.com
Find out more on the Accelerate website
Royal College of Podiatry The Royal College of Podiatry exists to ensure the public has access to high quality foot care delivered by qualified and regulated professionals.
Contact details
020 7234 8620
reception@rcpod.org
Find out more on the Royal College of Podiatry website
Diabetes UK Diabetes UK are the leading UK charity for people affected by diabetes it’s their responsibility to lead the fight against the growing crisis. And this fight is one that involves all everyone – sharing knowledge and taking diabetes on together.
Contact details
0345 123 2399
helpline@diabetes.org.uk
Find out more on the Diabetes UK website
Tell us what you think
If there’s anything you want to ask us or tell us, whether it’s a suggestion about our website, a complaint, or a compliment, drop us a line at
support@legsmatter.org









